In this article, you will learn how to safely manage medical devices with remote access. Remote access plays a pivotal role in supporting clinical operations by enabling technicians, vendors, and biomedical engineers to interact with devices without needing to be on-site. This capability is essential in today’s healthcare settings, where clinicians may be dispersed, uptime is non-negotiable, and rapid issue resolution can be the difference between safe care and catastrophic delay.
The case for secure remote access in healthcare environments
Organizations are embracing remote access for several practical reasons. First is the need for timely support; reducing mean time to resolution (MTTR) minimizes disruptions to care. Second is the reality of distributed healthcare, where equipment may be deployed across multiple campuses or patient homes. Third is cost efficiency: travel, downtime, and manual troubleshooting all introduce friction that remote tools can remove.
With this agility, however, comes serious risk. Medical devices differ fundamentally from general-purpose IT assets. They directly interface with the human body and handle protected health information (PHI). A compromise could leak patient data; worse, it could disable or distort a device’s intended function. This makes security controls around remote access not merely a regulatory checklist, but potentially a matter of life and death.
Understanding connected medical devices and their expanding role
The emergence of medical IoT (Internet of Medical Things) has transformed healthcare IT from a domain of computers and databases into a complex web of connected, often life-critical endpoints. Medical IoT encompasses any device that collects, transmits, or responds to patient data through a networked interface. This includes bedside monitors that stream vital signs to central dashboards, as well as telemetry-enabled pacemakers that sync with hospital servers during checkups.
Some of the most commonly connected devices now routinely managed remotely include:
- Infusion pumps: Adjusted remotely to modify dosage or flow rate.
- Ventilators: Tuned and monitored from afar to ensure continuity of respiratory care.
- Imaging systems: Accessed for remote diagnostics, software updates, or calibration.
- Wearable monitors: Deployed for outpatient care, syncing to clinical dashboards.
- Surgical robots: Maintained and updated by OEM technicians without local intervention.
These capabilities provide immense operational gains. Remote monitoring allows clinicians to detect anomalies early and intervene before a crisis. IT departments benefit from centralized oversight and more efficient maintenance scheduling. And from a systems engineering perspective, remote observability allows for better resource optimization across the device fleet.
However, with expanded connectivity comes heightened security concerns, especially with implantable or wearable devices. Pacemakers, insulin pumps, and neurostimulators have all been subject to academic or real-world vulnerability disclosures. In one well-known case, a security researcher demonstrated to a live audience the ability to intercept and alter his own pacemaker signals over unsecured RF interfaces, highlighting the life-threatening potential of such exploits.
Many of these devices use wireless protocols such as Bluetooth Low Energy (BLE), NFC, or Wi-Fi, each of which introduces its own risk profile. BLE, for instance, can be susceptible to proximity-based attacks unless pairing is securely managed. NFC offers a tighter range but weaker cryptographic protections in older implementations. Mitigation strategies must therefore include secure pairing protocols, minimal communication ranges, firmware hardening, and awareness of the physical environment in which these devices are used.
Threat landscape: What makes remote medical access risky?
The threats facing medical environments with remote access are neither theoretical nor rare. Healthcare systems are prime targets for cyberattacks due to the criticality of their operations and the high value of medical data. When remote access tools are misconfigured, undersecured, or over-permissive, they create footholds for attackers to compromise not just isolated devices, but entire hospital networks.
The most common threats include ransomware, credential theft, and unauthorized lateral movement. Ransomware campaigns like Ryuk and Conti have repeatedly targeted healthcare systems, locking out users from patient records and clinical systems alike. In many cases, initial access is gained through poorly secured remote desktop services or VPNs.
Legacy medical systems compound the risk. Devices still in active use often run outdated operating systems or proprietary firmware with little vendor support. Attackers exploit weak authentication, hardcoded credentials, and unencrypted communication protocols; that is, vulnerabilities that are often difficult to patch without affecting the device’s medical certification or a physical interface. The fallout of such a breach is twofold. Regulatory penalties under HIPAA, HITECH, and similar compliance frameworks can be severe, with fines reaching millions. More damaging still is the reputational cost: public loss of trust, operational shutdowns, and the ethical implications of harm resulting from compromised care.
Managing medical devices at scale
Managing connected medical devices across large environments requires consistency, automation, and security-conscious design. One of the most effective frameworks is zero trust architecture, which assumes that no device or user is implicitly trusted. Instead, each interaction must be continuously verified. In practice, this means authenticating every session, authorizing access based on current risk posture, and tightly restricting what each session can do.
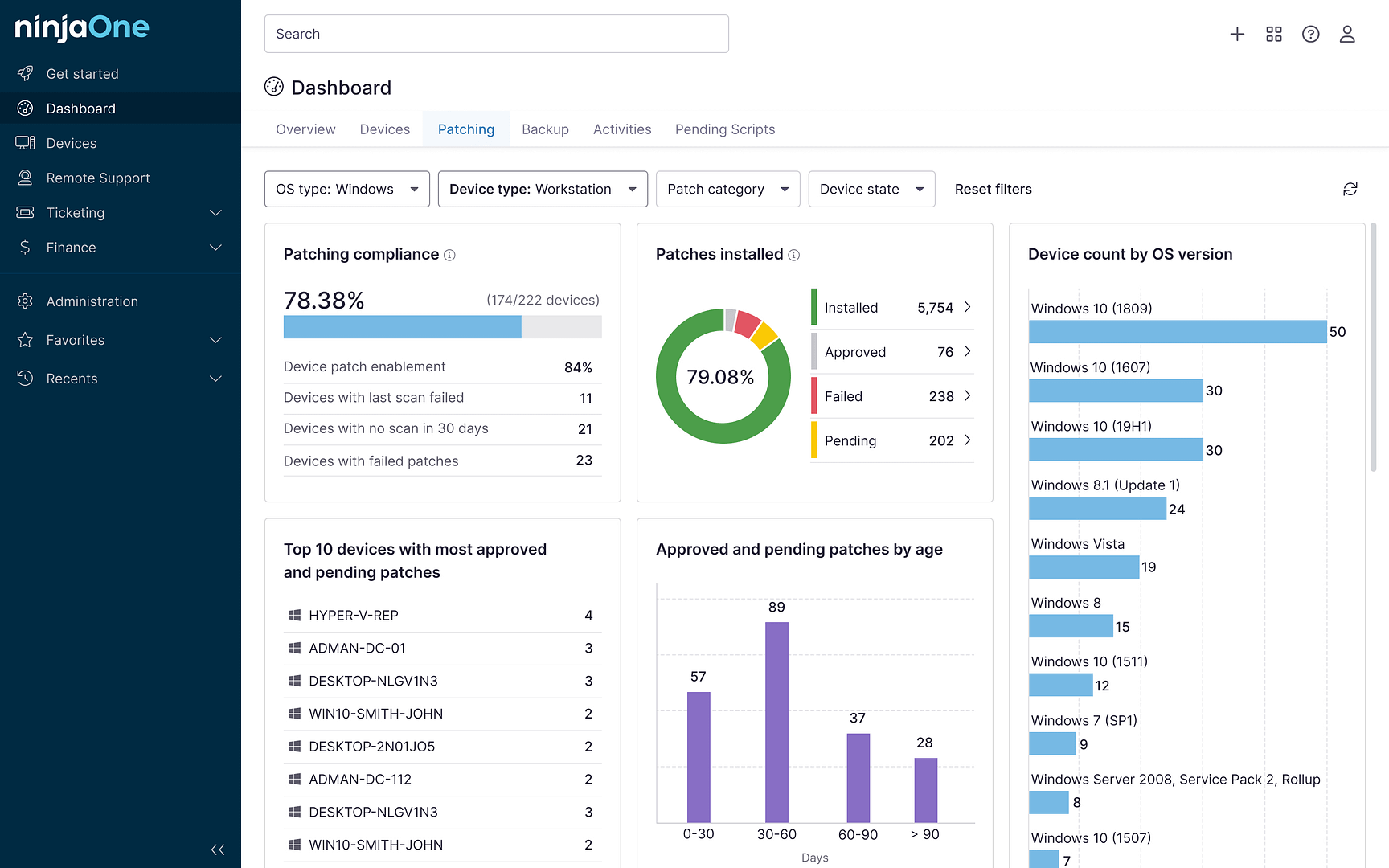
Choosing the right remote access tools is crucial. Traditional VPNs can be risky, particularly when used to access large internal networks without segmentation. Remote desktop protocols offer limited oversight and often lack granular permissions. By contrast, purpose-built secure RMM platforms designed for healthcare provide policy-based access, endpoint verification, and integrated logging – all designed to support both usability and compliance.
Patching medical devices is a persistent challenge, especially when uptime requirements prevent frequent restarts or changes. Automation can help coordinate patch deployment during approved maintenance windows, but only if it accounts for clinical availability and device interoperability. Testing updates in a staging environment is essential to avoid unintended side effects.
When things go wrong – as they eventually, inevitably will – several incident response plans must be ready. A robust strategy includes predefined workflows for isolating devices, communicating with clinical staff, and capturing logs for analysis. Monitoring systems should flag anomalous behavior in real time, allowing teams to intervene before incidents escalate.
Foundations of a secure remote access strategy
A secure remote access architecture begins with limiting the potential impact of a breach through a strong foundational design. The most effective way to achieve this is by segmenting networks so that medical devices are logically isolated from general IT infrastructure. This limits an attacker’s ability to move laterally from a compromised system to critical equipment. Secure architectures that emphasize compartmentalization and least privilege help constrain risk to only those assets directly involved in an incident, preserving operational continuity and patient safety even when a threat actor gains access to the network.
Encryption and secure communication protocols
All data exchanged with medical devices over a remote session must be encrypted using industry-standard protocols such as TLS 1.3, SSH, or modern VPN alternatives like WireGuard. Encryption ensures that sensitive commands and patient data remain confidential and tamper-resistant during transit, which is especially important when devices are accessed across the public internet or shared infrastructure.
Identity and access management
Managing who can access what, when, and how is a cornerstone of secure remote workflows. Implementing multi-factor authentication, enforcing role-based permissions, and rotating credentials on a regular schedule help ensure that only authorized users interact with clinical systems. Identity policies must also extend to vendors and support staff, whose access should be both time-limited and tightly scoped.
Logging, auditing, and remote session accountability
Every remote session involving a connected medical device should be logged in detail, including timestamps, user identity, accessed systems, and actions taken. These records provide crucial forensic data in the event of an incident, and also serve as a compliance control for frameworks like HIPAA and ISO 27001. Integrating session logs with SIEM tools allows for real-time alerting and pattern analysis.
Software bill of materials (SBOM)
An up-to-date SBOM allows healthcare organizations to track every software component, library, and dependency present in a medical device’s firmware or OS. When new vulnerabilities are disclosed, the SBOM helps identify affected systems quickly and enables targeted remediation. As software supply chain attacks become more common, SBOMs are emerging as a minimum requirement for safe long-term device operation.
Runtime security and threat monitoring
Security does not end once a connection is established. Runtime defenses such as telemetry collection, behavioral anomaly detection, and firmware integrity monitoring ensure that threats are identified even after perimeter controls have been bypassed. When integrated with a broader SOC or SIEM platform, these insights allow healthcare teams to correlate device-level activity with enterprise-wide threat signals and respond faster to emerging risks.
Navigating compliance: What the frameworks require
In medical environments, compliance is not optional; it’s foundational to both legal operation and patient trust. Secure remote access to medical devices must be implemented in a way that meets not just organizational policy but also specific regulatory expectations across jurisdictions. These frameworks don’t merely suggest best practices; many explicitly require technical controls for remote access, audit logging, encryption, and risk assessments. Staying compliant means building these requirements into workflows from the outset, not bolting them on after deployment.
| Framework | Scope | Key Remote Access Requirements | Notable Focus / Differentiators |
| HIPAA | U.S. healthcare entities | Access controls, audit logs, secure transmission of ePHI, periodic risk assessments | Focuses on patient data protection with flexibility in implementation |
| HITECH | U.S. HIPAA reinforcement | Breach notification, stronger enforcement, increased penalties | Emphasizes accountability and incentivizes adoption of secure practices |
| FDA Postmarket Guidance | U.S. medical device manufacturers | Vulnerability monitoring, coordinated disclosure, and timely updates | Lifecycle responsibility beyond device deployment |
| NIST SP 800-53 | Broadly applied in federal IT systems | Role-based access, encryption, system hardening, and session auditing | Control catalog that aligns with zero trust and high-assurance models |
| ISO/IEC 27001 | International information security | Policy governance, risk management, access restriction, and security incident handling | Widely recognized across industries, supports audit-readiness |
| IEC 62304, ISO 14971, UL 2900-2-1 | Medical device software and safety | Secure software development, risk analysis, and certified testing | Specific to device design and embedded software security |
Enabling technologies and trusted tools
Choosing the right tools for secure remote access in healthcare requires more than just technical compatibility. They must support compliance, provide visibility, and respect the operational constraints of clinical environments. This includes the ability to control sessions with fine granularity, monitor actions in real time, and maintain forensic-quality records of every remote interaction.
Remote monitoring and management platforms designed for healthcare deliver these capabilities by integrating authentication controls, role-based access, and session recording into a unified interface. Their ability to streamline vendor interactions and provide traceable access is especially valuable in environments where multiple third parties support equipment fleets.
At the endpoint level, protections must compensate for the limitations of embedded systems. While traditional antivirus may be infeasible, healthcare IT teams can apply safeguards such as configuration lockdowns, digital signing enforcement, and alerting for unauthorized changes. These help reduce attack surfaces without interfering with device performance.
Vendor access poses another layer of complexity. Biomedical contractors and OEM technicians often need privileged access, but must be managed with the same rigor as internal users. Effective solutions include dedicated vendor portals, time-bound credentials, and monitoring of vendor activity for signs of abuse or policy violation.
Security standards such as IEC 62443 and ISO 14971 offer frameworks for building secure-by-design medical systems. Aligning procurement and operational processes with these standards helps ensure long-term safety and compliance, particularly when working with new devices or custom-built platforms.
Lessons from the field: Case studies in secure remote access
While many risks to medical implant security are still emerging, several incidents over the past decade have already demonstrated the feasibility of attacks against real-world devices. These cases span from independent security research to public demonstrations and vendor advisories. Each incident reflects how predictable flaws can open pathways for potentially life-threatening exploitation:
| Incident | Device | Outcome | Readiness Level | Context Summary |
| Medtronic pacemaker hack | Pacemaker | Malware-enabled remote control of cardiac devices | Demonstrated | Researchers exploited the update toolchain to load unauthorized code onto pacemaker programmers, which could then be used to interfere with implant operation. |
| Barnaby Jack’s demos | Insulin pump, pacemaker | Wireless triggering of fatal insulin release and heart shocks | Demonstrated | Public demonstrations proved that some implants could be manipulated without physical access, exploiting unencrypted RF protocols and lacking authentication. |
| Medtronic MiniMed vulnerabilities | Insulin pump | Remote execution of overdose commands | Demonstrated | Researchers developed a proof-of-concept Android app capable of exploiting vulnerabilities in pump communication protocols to issue dangerous insulin dosages. |
| Jay Radcliffe pump hack | Insulin pump | Remote alteration of insulin delivery | Demonstrated | A diabetic security researcher exploited his own pump on stage, showing how a lack of encryption allowed unauthorized command injection. |
| Brainjacking concept | Neural implants | Theoretical risk of unauthorized control over neural stimulation | Theoretical | Researchers raised concerns that brain implants with wireless interfaces could be hijacked, potentially altering behavior, perception, or motor control. |
These incidents make clear that the attack surface for implantable devices is neither theoretical nor confined to future speculation. Device integrity, authenticated communication, and secure software lifecycles mustn’t merely be treated as technical issues when life or death can be at stake.
Ensure accurate records and safer outcomes. Watch Why are data standards important in healthcare.
Building resilience through remote visibility
Remote access to medical devices will become even more integral as healthcare decentralizes and care delivery extends into homes, clinics, and mobile environments. To stay ahead, healthcare IT teams must combine automation, continuous monitoring, and access orchestration in a unified approach that scales with demand and complexity. NinjaOne supports this evolution by providing a secure RMM platform for managing medical devices at scale, with built-in access control, telemetry, and compliance-ready reporting.
Try a free demo today to explore how NinjaOne can help future-proof your remote access strategy.